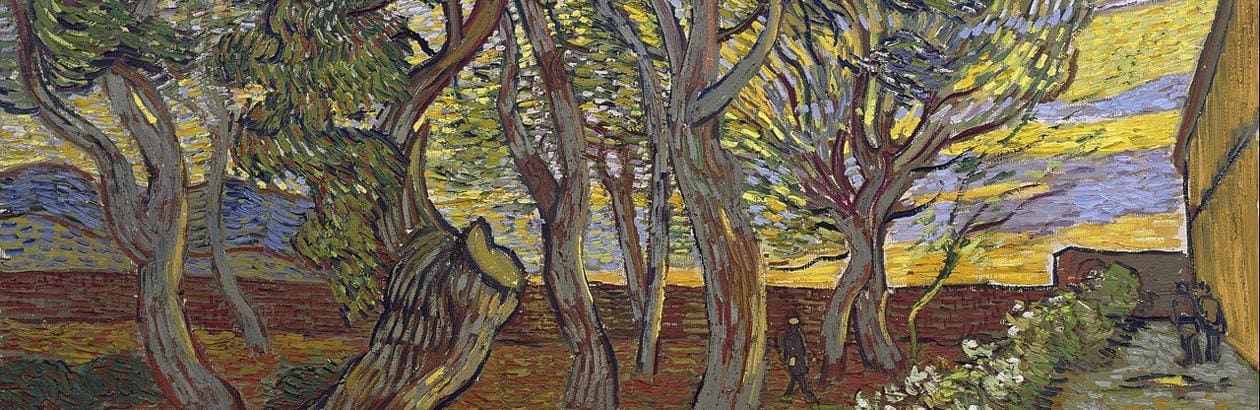
A
The beauty
of convalescence is the discovery that stillness
is a form in need of recovery
in which time repairs itself.
—David Bergman
A few weeks into medical school our dean asked us to perform a “time autopsy.” Having just begun to dissect our cadavers, we were asked to dissect our days—splaying out the “available” 168 hours of the week on a whiteboard before moving them around like chess pieces. While this proved a useful “time-hack” to maximize study, it also foreshadowed a strained relationship with time. In medical training, we were offered techniques for five-minute chair yoga, three-minute gratitudes, and six-second stress breathing. At its most nauseating, I was encouraged to take heart that only forty seconds of compassion were necessary for the patient to find my empathy “effective.”
Once in residency, time was fully commodified. As Neil Postman writes, “In the eternal struggle between God and Mammon, the clock quite unpredictably favored the latter.” As the pandemic made telemedicine routine, we were nudged to draw out five-minute telephone visits across a billable threshold of six minutes. Our notes closed with obscure timestamps like “greater than 50 percent of this twenty minute visit was spent in consultation with the patient.” Once in consultation with the patient, I was trained to set temporal boundaries: “We only have time to discuss one problem today.”
I was barely out of training before I began receiving frenetic promotions for telemedicine platforms promising to reduce my work time so I could see more patients and generate more revenue “immediately.” Through clinical machine-learning, I could quickly churn though “low acuity asynchronous visits . . . amounting to ten visits in one fifteen minute block.” One platform proudly boasted reducing “a single visit to 89 seconds of physician time.”
At last, by embracing hybrid time, the rushed clinician might enjoy the kind of lucrative, “asynchronous care” we all hope our loved ones will receive. “Asynchronous” is a perfectly unsettling word, meaning “not concurrent in time,” “misplaced,” or “belonging to a different time.” I think of physician Kenneth Bird, who coined “telemedicine” in the late 1960s and drew on media philosopher Marshall McLuhan: “Time has ceased, space has vanished . . . ours is a brand new world of all at onceness.”
Time is what Wendell Berry calls a “limit-in-ambush” that makes clear the boundaries of possibility in work—limits often hidden until that work has begun. “The making of any good work of art,” Berry writes, “depends, first, upon limits of purpose and attention, and then upon limits specific to the kind of art and its means.”
Healers claim to practice not just a good work but an art. There is something of an aura around the so-named “art of medicine.” But for the art of medicine to be both an “art” and a “good work” requires recognition of the limits of purpose and attention specific to the kind of art medicine is. One of these limits is time. The more medicine resists time as a limit-in-ambush, the more clinicians report a dissonant sense that “I didn’t have time to do what I needed to do,” and the more patients report, as a patient put it to me after a rushed encounter with another doctor, “nothing happened.”
Structuring visits such that patient and clinician make the most of limited time has always been a skill specific to the art of medicine. But modern health care has fostered new temporal responsibilities that make this increasingly difficult. For instance, the electronic health record, initially imagined as a time-saver, has actually increased time spent in both documentation and clinical work since its implementation.
As patient data becomes more automated, the sensory skills of the clinician—touch, hearing, perhaps even the temporal sense—become less relevant. Protecting time becomes as unnecessary as protecting physical presence. Instead, medical trainees turn their attention to algorithms, primarily as efficiency tools to save time. Researchers attribute this trend directly to high-volume, high-turnover clinical contexts, which habituate “treat and street” approaches that distance trainees from critical aspects of diagnostic reasoning and the trust-building practices needed for relationship.
One of ambulatory medicine’s leading challenges is reconciling the experience that comes with high volumes and the time required to care for those volumes, especially patients living with disability, complexity, or chronic illness. Here Mammon is especially insidious. Fee-for-service reimbursement rewards volume rather than outcome, prompting recent calls to align economic incentives to reward not just outcome but diagnostic accuracy and timeliness.
Less time with more patients pressures primary care clinicians like me to become “referralists” rather than practicing the comprehensiveness of training claimed, at least in theory, as generalists. Seeing patients at a rate of 3.8 an hour—roughly 30 a day—has been associated with higher rates of referral—a disconcerting observation given average wait times to see specialists are also increasing, suggesting a kind of congestive feedback loop in which generalists, who don’t have time to care for the whole person, are pressured to refer out more often to specialists, who themselves struggle to accommodate patients in a reasonable time.
Medical outcomes data from the late 1980s suggested that the best doctor-patient relationships and decision-making practices correlated with seeing fewer than 70 patients a week—about 14 per day—very different from the 25 to 30 today’s primary care clinicians are trained to see daily. And yet, when surgeon general Vivek Murphy analyzed the habits of seventeen “master clinicians” in 2015, each described high clinical volumes as critical to their formation: 60 patients a night in the emergency room, 30 patients a day in the outpatient setting. I think of my late grandfather, one of the first family physicians when the specialty was created in 1969, and this letter he wrote to my grandmother as an internal medicine resident in 1961:
I am on call today and have really been busy!! . . . I had to see most of the patients (at least 30–40). Besides which I had two admissions—one was a 2 week old, [the other] a 40-year old spry-and-chipper referred in for thoracentesis with a diagnosis of cancer of the splenic flexure. . . . I did tap and got off 500cc of bloody fluid. Also had to deliver a baby in my spare time. . . . Se-la-quere—it certainly is a variety and a challenge.
One gets the sense my grandfather was more clearly able to practice within his limits of purpose and attention. He was busy, to be sure, but with palpable joy. He clearly loved the medicine and the time.
The Music of Medicine
He also loved jazz. His love letters to my grandmother are riddled with lyrics. Growing up, he would answer questions by bursting into Sinatra. His love of music and medicine has helped me recognize time as a moral limit.
To illustrate this, I like to play Dave Brubeck Quartet’s jazz classic “Take Five”—but a condensed, twenty-one-second version I compressed in a music-editing software program. It always feels a bit awkward and gimmicky to play this brackish, shrieking clip—but it illustrates a truth better in sound than I can in speech: modern medicine often feels like trying to speed up a favourite song. In rushing a temporal art, medicine can become just as incoherent, forced, and carnival-like as compressing “Take Five” to squeeze it into an article on music and time. What we hear is not “Take Five” but something else—something shrill and uncomfortable that no one would recognize, let alone enjoy.
Modern medicine is relentless in its desire to cut apart, categorize, and instrumentalize, ever turning beauties into bullet points.
I’ll note here that despite growing up training in art and playing some music, I’m fearful of contributing to the health humanities’ tendency to gloss medicine’s challenges with the metaphors of art without catalyzing a change in the actual care of patients. Modern medicine is relentless in its desire to cut apart, categorize, and instrumentalize, ever turning beauties into bullet points.
That said, musical motifs have a particularly powerful way of shaping what we think is possible. Proust writes in In Search of Lost Time that music offers “actual ideas, of another world, of another order.” Musician and theologian Jeremy Begbie is a clear leader here, wary as he is of the “over-played half-truths” of musical metaphors, arguing instead that music, “in and through its making,” makes known the “temporal realities of the world”—a troubling observation considering music is consumed at a higher rate than ever before, while fewer and fewer actually make it, raising the question of whether, in a visual culture driven by the screen, we are losing the eyes to see (or rather ears to hear) the temporal realities of the world.
There is an interesting parallel in medicine. While clinical notes are generated at a higher rate, fewer of them are actually read. The very notes clinicians type with hurried hands and the rushed encounters they experience echo Roger Scruton’s complaint that much modern music-making no longer features melodies written to convey a story so much as scraps of melodies cut short, condensed, and copied forward. It is relatively easy to find a discrete piece of data in the electronic health record. It is quite another matter to gather a coherent sense of a narrative, story, or indeed a timeline.
This temporal industrialization in medicine already has a long line of resistance in the “slow medicine” movement started in the 1980s, made most famous perhaps by the work of physician Virginia Sweet and theologian John Swinton, who beautifully attend to time’s limit-in-ambush in hospice, palliative, and disability care.
I recognize my emergency and surgical colleagues operate under different temporal constraints (“time equals tissue” as they say). But even there, as surgeon Huma Farid writes, like a song, “an operation cannot be hurried along.”
Music has helped me see that healing medicine’s broken relationship with time is not merely slowing down but seeking the right time. Musicians call this the tempo giusto—“the right speed”—what physician Delese Wear and her colleagues suggest is a critical but neglected aspect of “slow medical education.” The tempo giusto can be understood as both “ordinary time” and “ideal time.” It simultaneously captures the perfect time always out of reach and the ordinary, quotidian time one plays and practices within daily.
Thinking about tempo giusto has helped me wrestle with what is often misconstrued as a call to doctors to just slow down. Some of the best jazz solos are well-worn melodies compressed, inverted, or re-arpeggiated across different time signatures with temporal demands that might otherwise be thought impenetrable. Begbie notes that “music, by its very constitution, can serve to release us from the assumption that limited duration is of necessity problematic, that we can only discover authentic meaning in the unbounded and unlimited.” To play my compressed version of “Take Five” renders it unrecognizable in one sense. But in another subversive sense it offers, as my grandfather wrote about his patients, “a variety and a challenge.” It is a mystique of the jazz tradition that the masters emphasize the challenge of the unexpected. The best jazz does not offer an easy resolution. As the drummer Leroy Williams said, “It has to do with where you put your accents when you’re improvising.”
Making Margins
But I don’t want to suggest that the temporally inured should just learn better improv. Time is a moral limit-in-ambush. At some point improvisation is wheel-spinning more than generative. It seemed a fitting omen that the music recording program I used could not compress “Take Five” below ten seconds without crashing. The analogy in medicine is painfully obvious: the more patients we try to fit in less time, the more likely the system is to crash. The more likely patients will feel compressed and clinicians will burn out. As former internal medicine residency director at Massachusetts General Hospital Jay Vyas recently put it, today’s trainees endure a “compression of time” and turnover worse than the generations of doctors before them—and this after decades of medical educators experimenting with new ways to accent the training.
An old jazz pianist friend of mine (whose own music wrestles with time) once encouraged me to read Scripture this way, listening for where ideas echo within the text. I think of Nehemiah in the Old Testament book of the same name. The Jewish people are under Persian rule. Their temple has been rebuilt but lies unprotected—in need of walls. Nehemiah has been serving as a cupbearer to a foreign king, Artaxerxes I, for years. The story captures Nehemiah as one forced into a tyrannical system, serving a master he does not want, while waiting, watching, and listening long before boldly and prayerfully asking for permission (and funding) to build something new.
It happens weekly it seems—a patient will tell me something painful, something it takes a long time to say. It is as if I must demonstrate a willingness to serve slowly before the patient will offer the necessary diagnostic clue or hidden suffering they’ve never revealed. But this requires time. It is the limit-in-ambush of primary care, where the word “patient” bears out both its definitions—to suffer and to wait.
Philosopher James K.A. Smith names this as one of the “scandals of temporality”: “Insight tends to crystallize at the end of things,” and “discernment is a core virtue of temporal faithfulness.” In primary care, that temporal faithfulness is often hard-won—serving even within temporally oppressive systems. But it also might mean a big ask to those in power, leaving one structure to build a new one. As Nehemiah 2:6 says, “So it pleased the king to send me, and I set a time.”
What kind of temporal margin is necessary to see, let alone serve, the suffering on the side of the clinical road?
But what if waiting is not possible? In “A Pervasive Culture of Time Constraints in Health Care,” physical therapist Hannah Todd points to a research study in which seminary students were told they needed to go to another building to give a talk about the good Samaritan. Half the students were told to head over, while the other half were told to hurry because they were already five minutes late. Each student encountered a man slumped over in the hallway. The rushed students only helped 10 percent of the time, while the other students helped 60 percent of the time. One question this raises is what kind of temporal margin is necessary to see, let alone serve, the suffering on the side of the clinical road.
Twenty years ago the primary care physician Richard Swenson diagnosed patients with “a new disease” he called “marginless living,” which he attributed bluntly to a “lack of love”—interesting considering John Swinton’s call for gentle timefulness sets the pace at “the speed of love.” For Swenson and Swinton, having enough margin is not just a temporal privilege but a loving act of architecture. If Nehemiah inspires new temporal walls, then it seems the Samaritan inspires gates and battlements—rests in the musical score.
In a review of the band Polyphia (very much a group with a virtuosic command of tempo), guitar teacher Michael Palmisano advises, “Forget about just thinking about space as far as silence. . . . Yeah, the funk is in the silence . . . but using, taking away silence, adding things in . . . is crucial.” One example is the fermata—“the hold” or “grand pause” that can indicate both a note held beyond its natural duration or a short interval of silence. Like the tempo giusto capturing both the ideal and the ordinary, the fermata suggests a posture willing to linger or leave. As Sharon Pretti writes in her poem “Surgeon,” “When she returns him, / she stays with us longer / than she has to, taps / her thumb on the / stethoscope’s disk—lingers, / as if she wants to say / where she’s been, the part / of him cleaved to her palms.”
I think of another healer with marked palms who was willing to linger. In John 11, Jesus will not be rushed at the death of his friend Lazarus. The urgency of Mary and Martha’s plea—“if you had been here”—is counterbalanced against the apparent delay of the One who is never late, who upon hearing that Lazarus was ill, “stayed two days longer in the place where he was” (John 11:5). The King James reads “he abode two days still,” suggesting a deep mastery of time in which Christ waits, walks, and weeps before waking Lazarus—which he does “in a loud voice,” phōnē, “as of a musical instrument.”
As a family doctor who has been formed to treat time like another lecture to listen to at 2.5× speed, these three stories inspire me because they capture a moral relationship with time that is abundant and generative rather than scarce and white-knuckled. Nehemiah, the good Samaritan, and Christ himself live as if they have enough time. And as Smith writes, “Having enough time is an act of hope.”
Having enough time in medicine—at least, in primary care—is an act of hope because it changes what one expects from time. It seems to say, “I recognize that the fulfillment of this good work we call healing requires a temporal depth that points beyond what I can fit into the brevity of my one life.” It is like Arthur Hertzler, “the horse and buggy doctor” of the early 1900s, who wrestled with the strange realization that—given medicine’s iterative nature—50 percent of his work would be written over by the next generation. The remaining half was just presence to the one who suffered—cold sponges on the brow of the feverish, long forgotten in the hidden hours of the night.
A Time for Hope
The very act of music-making is similar, as the majority of musical compositions are never heard or even played. I spent some time in an indie rock band called Real Work—yes, after Wendell Berry—and one of my favourite parts of this experience was encountering truly gifted singer-songwriters who could easily “make it” but were unlikely to ever break out of the no-name dive bars we were playing in. Theologian Ephraim Radner points out that this is a moral problem that confronts not only what we think about the purpose of art but also what we think about hope. If music is meant to be heard, it seems tragic when it is not. And yet so much of human art and love is this way—harmonies sung by families that will never be recorded or monetized. Mothers feeding their little ones in the dark. Anthropologist Douglas Christie argues it is precisely this willing descent into obscurity that is the paradoxical path in which caregivers might practice the kind of hope and timefulness necessary to become “bearers of compassion.”
In medicine, the very act of welcoming a patient is a hopeful act, for it entails the reasonable expectation of healing or some measure of future relief. But given hope’s orientation toward something that has not yet happened, it also entails a kind of willing risk of disappointment—what J.R.R. Tolkien called “hope without guarantees.” It holds open a future of irresolution, in which accompaniment and bearing compassion may be all that is possible for the one who continues to suffer. Immunologist Brittany Bettendorf calls having the time to listen the last hope for the art of medicine.
But it doesn’t take long in medicine to realize that “Parkinson’s law” abounds—the work fills the available space. Even when one builds walls and margins and seeks to have enough time, it can be challenging to maintain hope when those new margins quickly fill to become new burdens. We need examples of those who can apply new temporal postures in lasting ways. As Harvard cardiologist and chief medical officer Thomas Lee said in an interview, “You have to make decisions that wouldn’t make sense to the CFO.”
I work in a direct primary care practice that has tried to inhabit a musical relationship with time. My colleagues came up against time’s limit-in-ambush after serving in high-volume medical centres and outpatient clinics for years. In prayer and attention to their patients they discovered, like Nehemiah, the hope to leave a temporally oppressive system and build something new.
We charge patients a monthly membership fee that is less than the average cell-phone bill. Because we don’t go through insurance, we are not beholden to the incentives or requirements that drive high volumes and shorter visits. Our time with patients speeds up or slows down relative only to the needs of the patient. We try to practice at the speed of love, prioritizing availability, presence, and attention.
A core conviction of our practice is recognizing both patient and practitioner as ensouled creatures with limits. Like a song, suffering cannot be hurried along. We have margin to admit our own patients and follow them in the hospital. We can accommodate the acutely ill, linger with the disquieted, make house calls, practice pro bono, and treat patients with tempo giusto—the right time. If a patient has a common cold, we don’t force the visit to expand into twenty minutes if a quick consult is fitting—but we have the time to linger, asking if there is anything else they might want to say, protecting that great mystery of the art of primary care, in which sometimes even a common cold can be the entry point into a deeper wound that requires more time.
I recognize that this model of primary care will not be found compelling, coherent, or just by all medical workers. But it has given me hope for recovering primary care as a work of art—good because it honours the limits of purpose and attention specific to the art of general medicine. I have found, in my admittedly brief time out of residency, that I can care for my patients slowly and thoughtfully, which I never thought I would be able to say after years of being trained to prioritize efficiency above all, working as quickly as possible and therefore always at risk of what philosopher and physician Jeffrey Bishop calls “thoughtless doing.” We can practice what an attending once told me is the most neglected elixir in primary care, “a tincture of time.”
Direct primary care is not a panacea for healing the doctor’s strained moral relationship with time—nor does it automatically create margin for the marginalized, answer the temporal challenges of my subspecialist colleagues, or offer counsel for the medical trainee who carefully titrates her morning to see all her patients before rounds. I have not forgotten what it is like to literally time the duration of my bathroom breaks and documentation habits in a desperate attempt to squeeze one more second of control out of the day. After all, Aslan himself urges Lucy to hurry as she tends to the wounded in The Lion, the Witch and the Wardrobe. I recognize haste may be the call.
As Smith puts it, “What counts as growth is pegged to this elasticity of time.” He goes on, “Don’t compare the trees of your tundra existence to someone’s else’s equatorial rain forest.” For medical trainees in particular, this might look like making a bid of temporal solidarity with the patient—“I know you feel rushed, I feel rushed too. How should we honour our time?” For medical educators, benefactors, and innovators, it may mean taking up the adventure of building houses of training and healing that keep pace with sacred, ordinary time—delighting in the variety and challenge and insane hope of having enough time.
Dave Brubeck Quartet’s “Take Five” comes from their album Time Out, a work that specifically wrestles with unusual time signatures inspired from Turkish street musicians. The title does not imply the easy solution of taking a five-minute break so much as finding the time when the beat is difficult and then making something new. A similar creative task is before primary care clinicians who feel time’s limit-in-ambush—listening long for the right time to build new walls of practice marked by hope and presence and the beauty of convalescence, a form of stillness in need of recovery, in which time repairs itself.